A data analysis conducted by researchers from Macquarie University under the auspices of the Australian Institute of Health Innovation using POLAR* data from three Victorian PHNs (Eastern Melbourne, South Eastern Melbourne and Gippsland) highlighted the extent of the decline in face-to-face visits at both GP practices and RACFs as a result of the COVID-19 pandemic lockdown and subsequent reduction in community movement throughout Victoria.
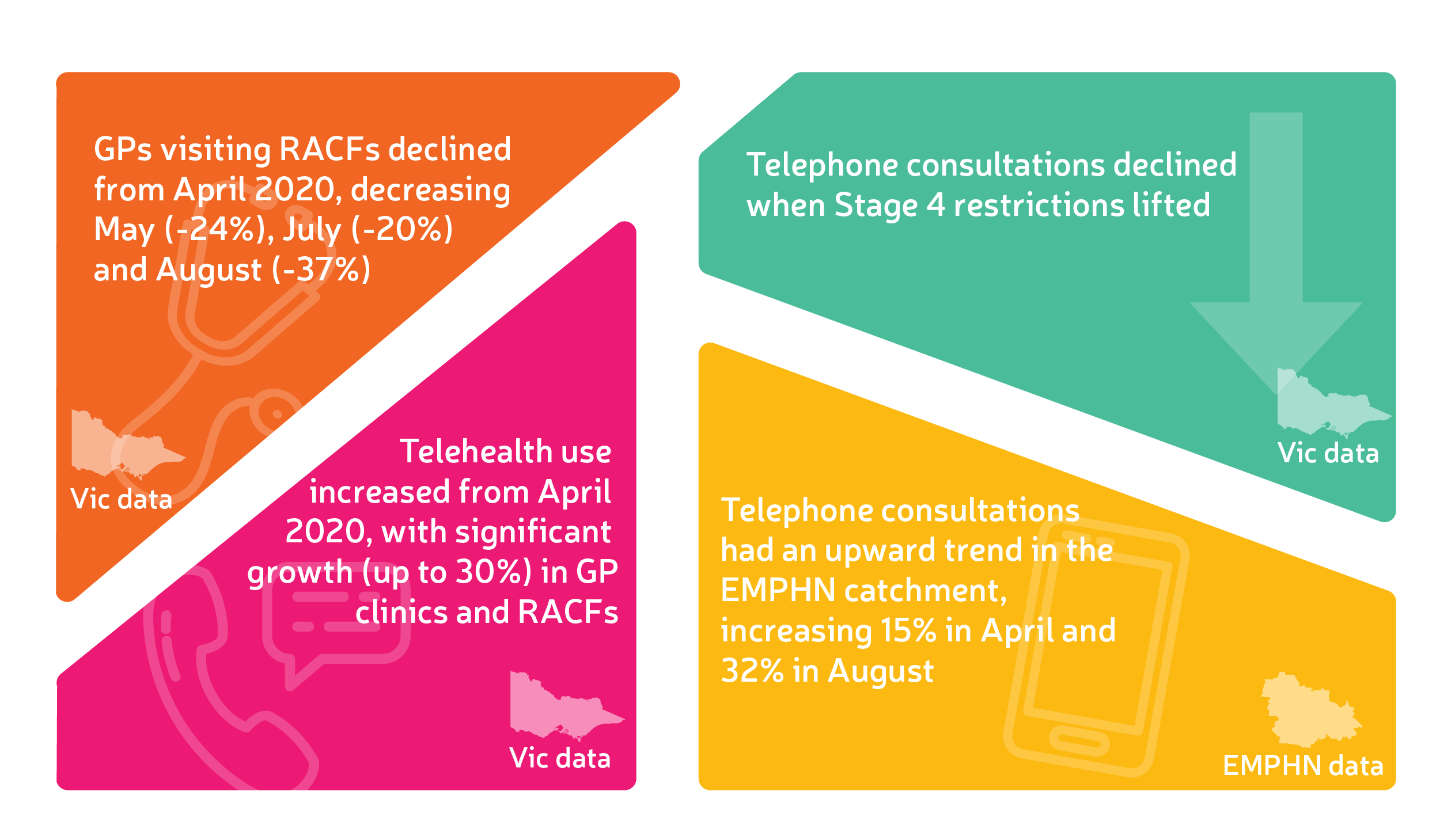
The decrease in GPs visiting RACFs face-to-face commenced in April 2020 and was most evident during the height of the pandemic lockdowns in May (-24%), July (-20%) and August (-37%).
The study showed a corresponding increase in use of telehealth during this time, with a significant growth in telephone consultations (up to 30%) for RACF and community GP consultations.
Key findings from the study included:
- Telephone consultations had an upward trend in the EMPHN catchment, increasing 15% in April and 32% in August
- Telephone consultations declined when Stage 4 restrictions lifted
- While video consultations increased in 2020 compared to 2019 there was no significant increase in its use throughout the key lockdown months, especially when compared to telephone consultations
- Barriers to use of video consultation technology include technology accessibility, poor connectivity, data security concerns and sound/image quality.
Dr Precious McGuire, a clinical advisor to EMPHN and a GP at Deepdene Surgery said the study was clear evidence for the need for ongoing MBS telehealth item numbers, beyond the current end date of 31 December 2021. Telehealth has improved access to general practice care for vulnerable patient groups including those residing in RACFs.
“The study clearly showed the value of telehealth across the entire network of GP practice, both in community consultation and within RACFs. Having access to this real time data helps us respond more quickly to emerging needs in our community and instigate changes to existing programs, inform new program design and advocate with evidence-based advice to the Department of Health."
EMPHN System Design Specialist, Shirmilla Datta, whose work on the study was cited by the authors in their final paper, said another important finding from the study was lack of data clarity within POLAR to allow for a ‘tick box’ to identify RACF residents separately from other patient cohorts, something that the Royal Commission into Aged Care Quality and Safety has recommended in both MBS and PBS datasets by mid 2022.
“While this information wasn't available to us for this study, it is something we can work on with the software developer for further insights into the aged care sector cohort. The more information we can elicit through POLAR and other means the better off our aged care program support can be.”
During 2020 almost 20% of EMPHN-based RACFs reported at least two cases of COVID-19, with several becoming hotspots. The data analysed came from 37 general practices within EMPHN’s catchment. The study snapshots can be viewed in full on EMPHN’s website.
*Population Level Analysis & Reporting (POLAR) is a web-based platform which uses de-identified clinical and population health data from general practice to provide insights that can be used to support improved programs and resources.