Eastern Melbourne PHN's (EMPHN's) 18-month Health Coaching program began in May 2019 and sought to enhance current capacity and support capability building within the Primary Care Nursing workforce to improve health outcomes and quality of life for patients with chronic conditions.
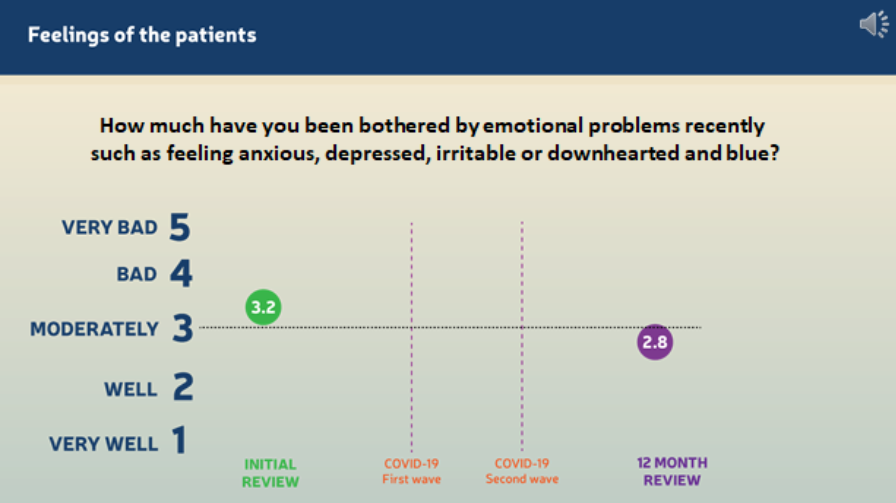
The overwhelmingly positive health and quality of life outcomes delivered and maintained by the Health Coaching program were unprecedented given the heightened stress, anxiety and emotional volatility experienced by many due to COVID-19 restrictions and lockdowns.
EMPHN facilitated the program rollout, working closely with Medicoach to deliver a suite of professional development workshops and mentoring sessions with the intention of building skills and enabling nurses to work effectively as health coaches, educators, chronic care managers and care coordinators.
In addition, EMPHN provided support for nurses to embed their new skills to drive positive, tenable behavioural changes in patients with chronic disease. To supplement the health coaching, access to an online patient education was provided by Heathily through their platform ‘GoShare’.
Twelve general practice clinics participated the program and each clinic nominated a nurse, who was supported by a general practitioner (GP) and practice manager (PM), to undertake the training and implement the program.
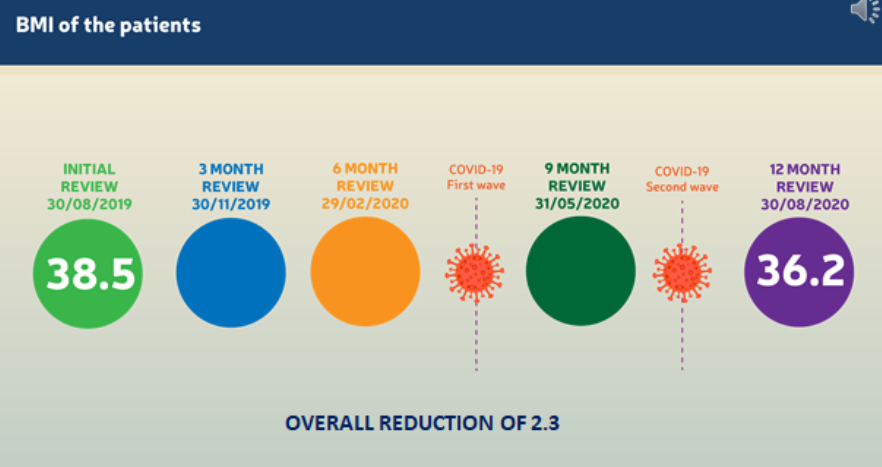
One-hundred-and-seventeen patients enrolled in the program with reviews carried out every three months. The following results were recorded by the 47% of patients who attended every review, over a 12-month period:
- average BMI improved from 38.5 to 36.21.
- responses to a survey question on being bothered by emotional problems (such as feeling anxious, depressed or blue) improved from 3.2 to 2.8, on a scale of 1-5, 5 being very bad2.
COVID-19 impacted the delivery of health care and the general health and wellbeing of individuals globally. It was anticipated physical distancing measures and restrictions would affect the ongoing delivery of the Health Coaching program through participation drop-offs, however the clinics and nurses mitigated this by quickly adopting telehealth and continuing to support patients and their ongoing participation throughout Melbourne’s two lockdowns.
EMPHN’s support for nurses included regular practice visits and virtual catch-ups, collection of de-identified data, access to GoShare, model of care planning and implementation, and problem solving for clinic-based integration and COVID-19 challenges.
Key highlights from the program as evaluated by nurses was the emphasis on making small changes, the importance of relationships in fostering change and the use of motivational techniques to encourage patient self-management in their health journey.
Allison Mason, a participating nurse from DPV Health Medical Clinic highlighted the importance of seeking only 1% of change, finding that little changes that were achievable and maintainable improved patient self-advocacy, confidence and readiness for change.
She said the program provided “tools to be able to talk the language that is required to get those 1% changes, to help advocate and stick to the goals that patient is making.”
Jean Lua, from Mediscreen Clinic said “throughout the program I was given all-round support that equipped me with powerful tools of communication and empathetic approaches, ways to empower clients to achieve their health goals and ultimately better quality of life."
"I feel this program not only gives the Nurse the skills, but also the confidence to be able to do more in the space of nurse-led clinics and chronic disease management alongside our GPs. This program was a way of showing GPs that there is an untapped resource there and highlighting the skills the nursing staff have to improve integration and effective health management." said Tania Worroll, a participating practice manager from Selby Family Clinic.
The Health Coaching program will continue to provide further training for nurses, ongoing support for existing patients and recruit more patients into the program in 2021.
References:
1 Average BMI improved from 38.5 to 36.2 over the 12-month period for 55 patients who attended every review.
2 Responses to a survey question on being bothered by emotional problems (such as feeling anxious, depressed or blue) improved from 3.2 to 2.8, on a scale of 1-5.